Dashboard Redesign
2016 -2017


Project Overview
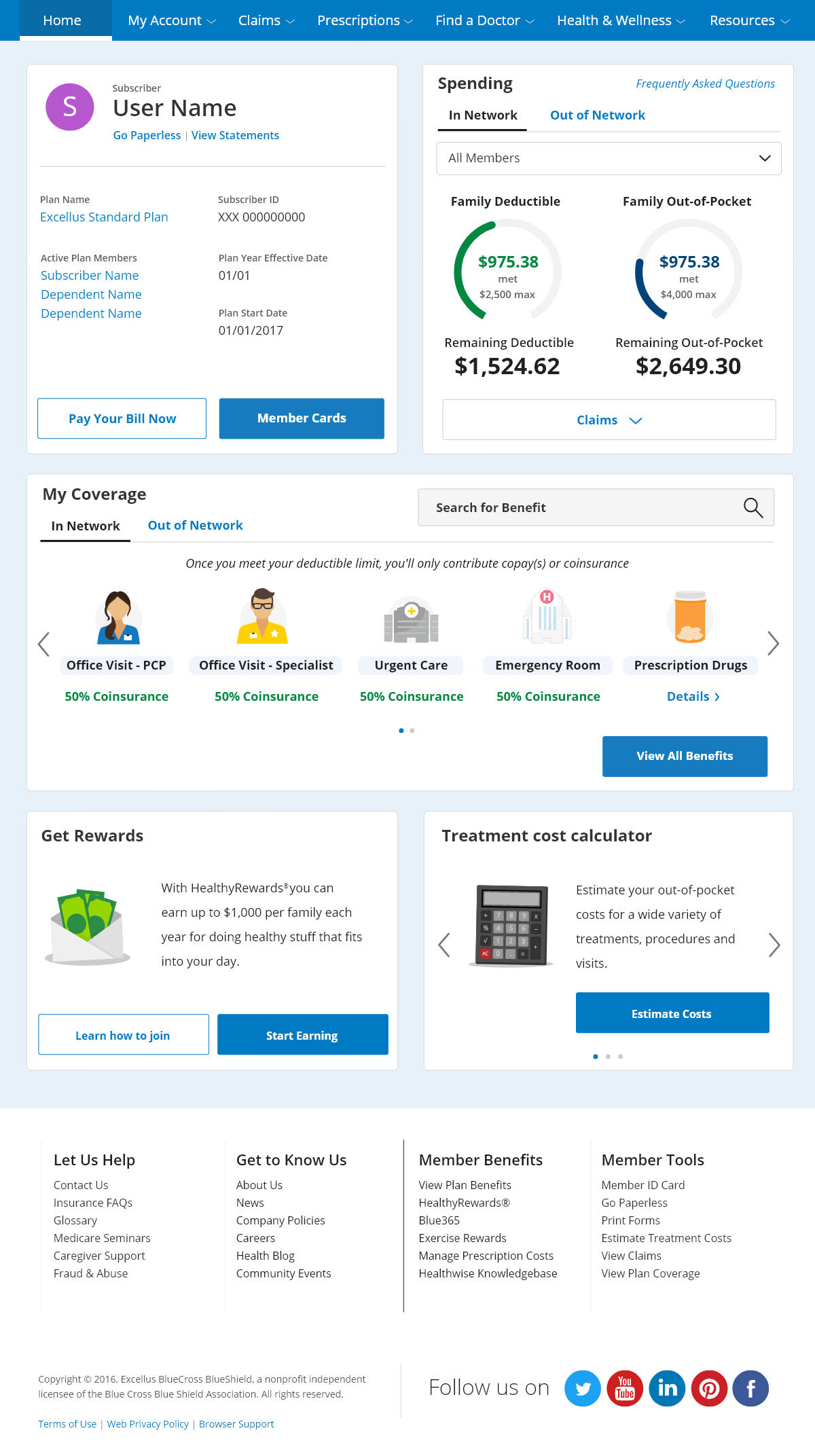
This was a board goal that involved a non-negotiable timeline. We were moving code from an existing platform to a new web platform while also redesigning the entire Member and Medicare member user experience. Upfront discovery and system requirements drove scope decisions before handing over project work to the UX/UI teams to begin work.
Our Users:
Our target users were all insured members of a health insurance company. We had to analyze the data around the current features, perform heuristics, and determine what was needed in the designs to accommodate the new, much larger population of members and dependents aged 16-100+. The first design had multiple usability issues such as not being accessible under WCAG guidelines.
Role and Responsibilities
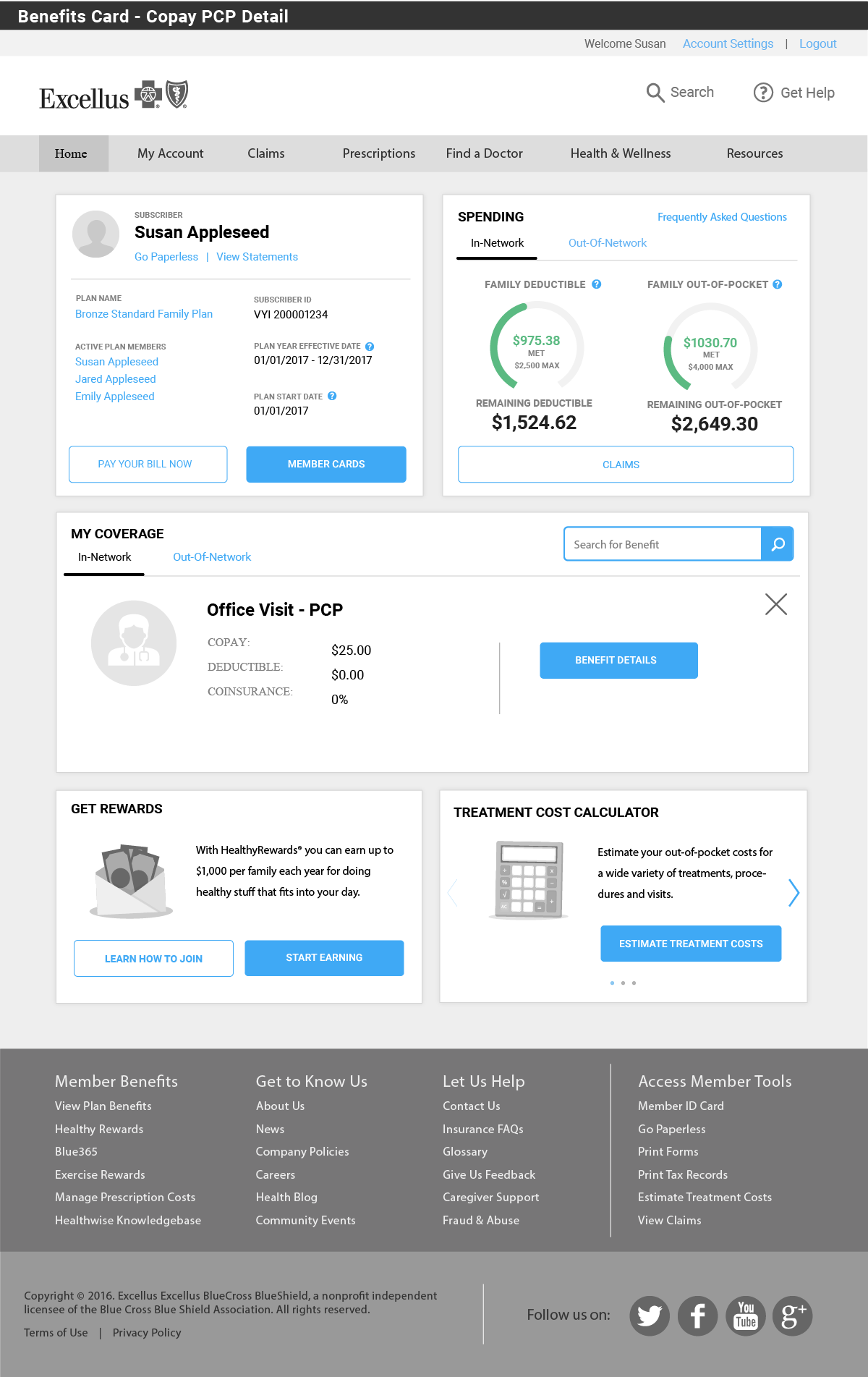
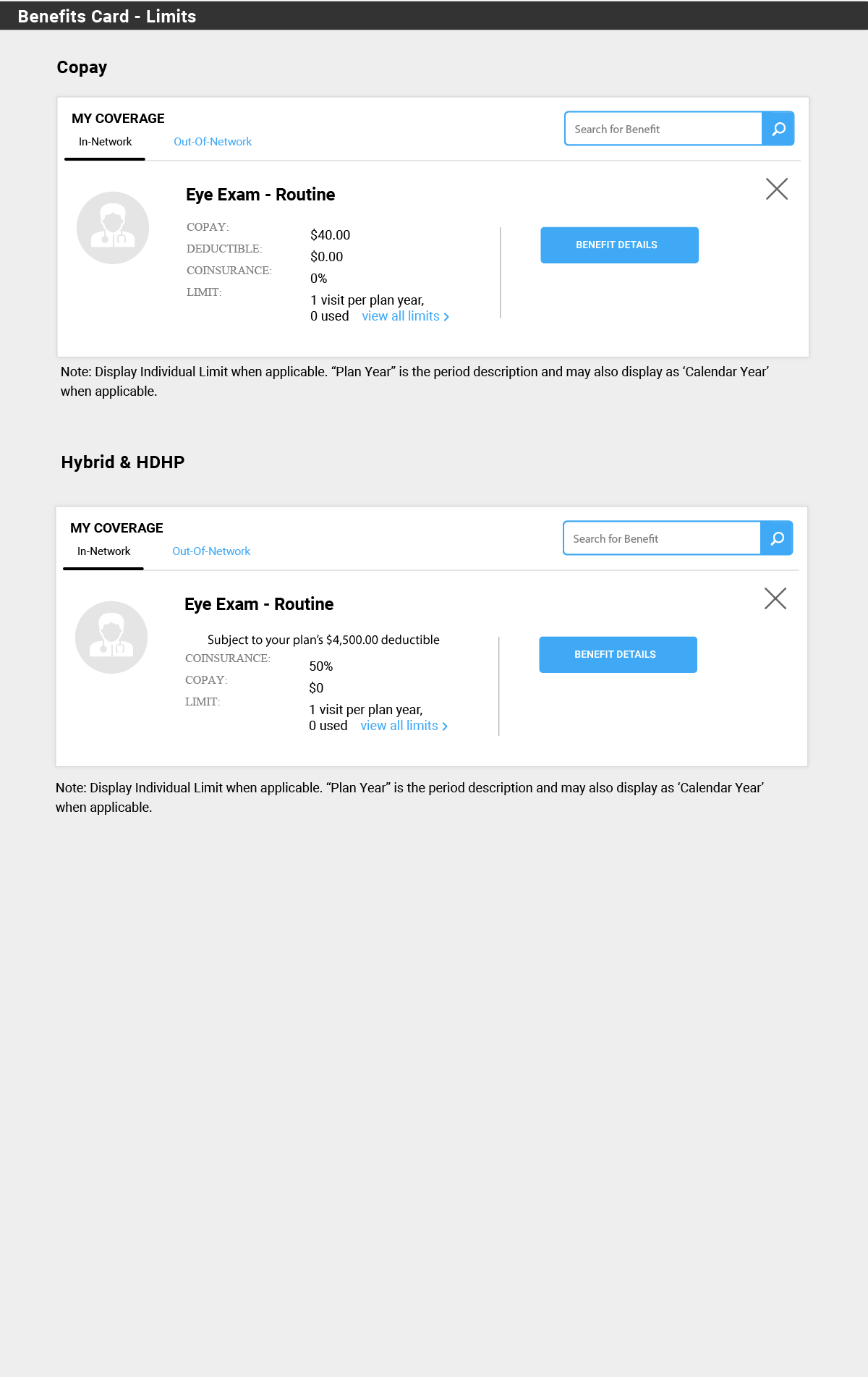
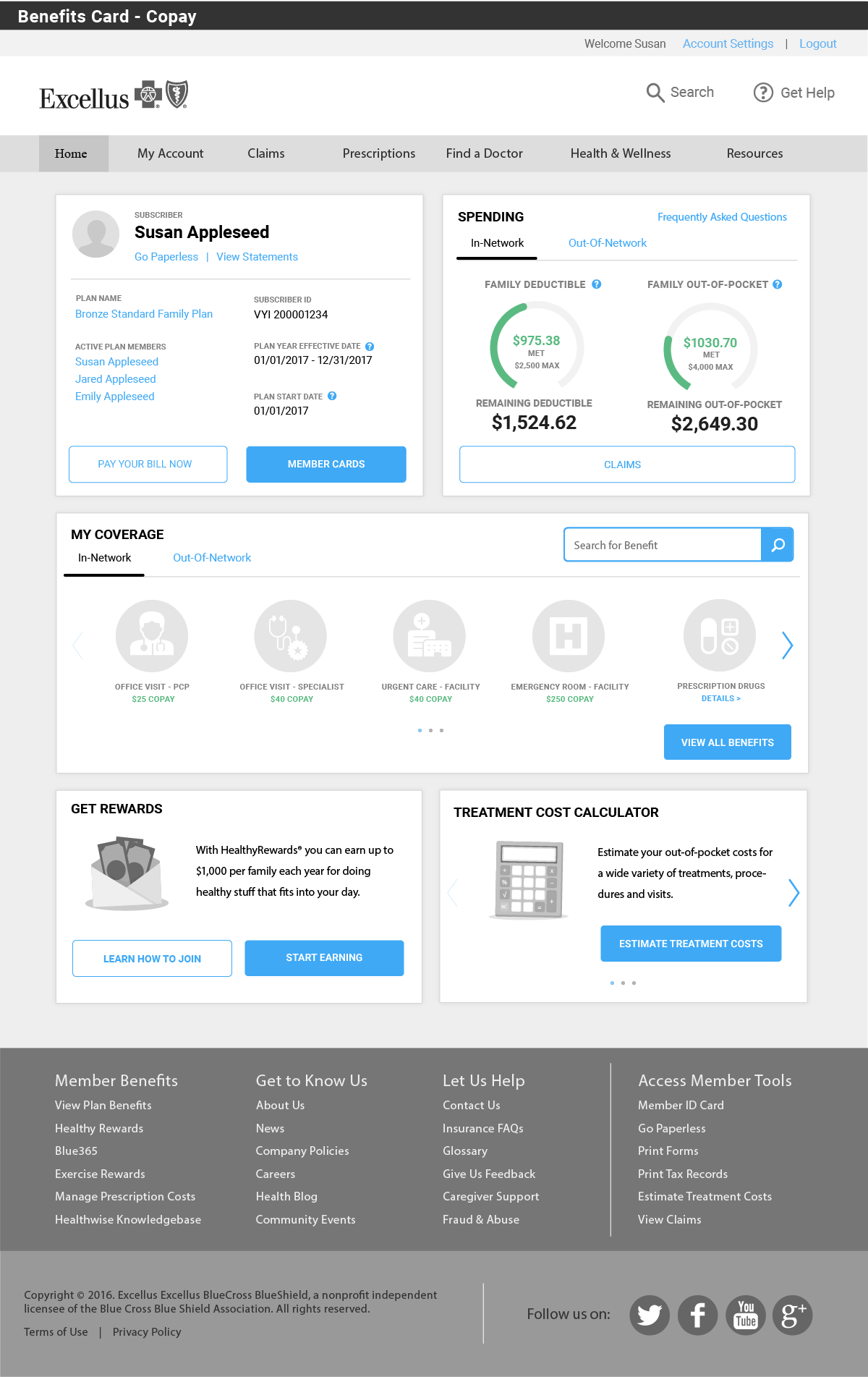
At the start of the discovery phase, I was part of the research team tasked with conducting initial user research, collecting and analyzing feedback, overall heuristic analysis, and IA summary reporting. Once scope was established and work was segmented out, I manly focused on creating the new UX designs for the Member dashboard along with any secondary pages. Initial wireframes were then put through two stages of user testing and user feedback was collected at each session.

Outcome
After final designs and UI development were completed, we were able to do a final round of selective "live" user testing. We launched to all members during the new Open Enrollment year of 2017.
We determined three avenues to track and mark success of the new designs; One, to all pre-existing APIs and portal functions were successfully brought over to the new platform and performed better than previous installments; Two, we interviewed, collected, and tracked initial user feedback of the redesign to meet a benchmark of 60%-70% overall improvement; Three, continue to track user feedback, while in parallel monitor our customer service center for incoming end user problems, and track them over a repeated three month, six month, and yearly review.